You don't have to suffer from uterine fibroids
Fibroids can be cured using a non surgical minimally invasive technique recommended by the National Institute of Clinical Excellence that typically takes one hour. The success rate is over 95%.

Uterine Fibroids can be cured by a non surgical
microinvasive 1 hour procedure
The procedure is explained at length on this website

On this website
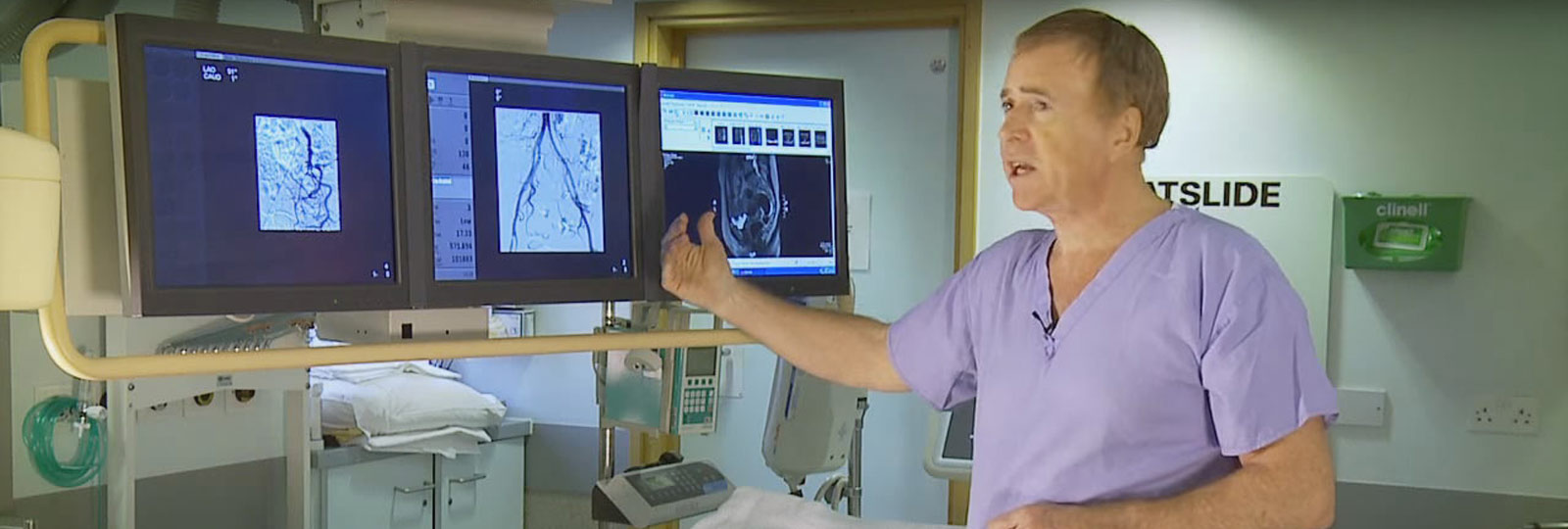
DR. W.J. Walker
presents information on curing uterine fibroids by Uterine Fibroid Embolization
Call Doctor Walker now for help and advice
Uterine Fibroid Embolization
The traditional treatment of fibroids over the years has been hysterectomy - but no longer
Read moreFibroid Embolization and Pregnancy
The trial at the Royal Surrey County Hospital and London Clinic represents the largest world series of pregnancies
Read moreFrequently Asked Questions
Dr. Walker answers the most frequently asked questions about fibroid embolization
Read moreAdenomyosis
Adenomyosis which may coexist with fibroids is a condition in which cells from the lining of the womb . . .
Read moreHormone Replacement Therapy
Fibroids are one of the contraindications to hormone replacement therapy (HRT) . . . .
Read more
ESMYA
Esmya is a medicine, which is supposed to be used only in the short term for control of fibroid symptoms . . . .
Read moreDelayed Treatment
prompt treatment should be strongly considered before the fibroids become too large . . . .
Read more
UFE IN Young Women
Sarah was 13 years old when her mother took her to her GP because she had fainted at school . . . .
Read moreMirena Coil and Submucous Fibroids
The Mirena coil has been a great invention that in most instances effectively stops women having significant periods.
Read more
Myths
Many women in their forties with fibroids causing significant often debilitating symptoms
Read moreAsherman's Syndrome
Asherman’s syndrome is due to fibrotic scarring in the uterine cavity called adhesions.
Read more
Media Coverage
Television, Radio and Newspaper coverage of Dr. Walkers's embolization experience.
Read moreHomeopathic
There is a concept amongst some of the public that natural cures are to be preferred to scientific ones.
Read more
Our Patients' Stories

More Information Regarding Self Funding
For more information regarding self funding prices at The London Clinic, Nuffield Health Guildford Hospital or any other private clinic contact Dr. Walker's Executive Assitant on 07795 643019 or via email: wjwalker@uk-consultants.co.uk
Procedures Performed
100% success rate
Successful Completed Pregnancies
Our Partners